When Your Body Bleeds From the Inside
Imagine trying to find a small leak in a long garden hose that's buried underground. You know water is escaping somewhere, but you can't see where. That's exactly what doctors face when someone has bleeding inside their intestines. The small intestine is about 20 feet long and twisted like a coiled rope inside your belly. Finding the exact spot where blood is leaking can be like searching for a needle in a haystack.
But recently, doctors discovered a clever way to solve this problem. They used a bright blue dye called methylene blue to highlight the bleeding spot, making it easy to see during surgery. This breakthrough saved a patient's life and could help many others in the future.
What This Story Is About
This article tells the story of how doctors used a simple blue dye to solve a complex medical problem. We'll explain what went wrong in the patient's body, why it was so hard to find, and how the blue dye made everything clear. Most importantly, we'll help you understand what this means for people who might face similar health challenges.
Why This Matters to You
Every year, thousands of people go to the hospital because they're bleeding somewhere inside their bodies. Sometimes doctors can find the source quickly. Other times, it's hidden so well that patients need multiple tests, surgeries, and treatments. This new technique could make the process faster, safer, and more successful.
A Simple Solution to a Complex Problem
The beauty of this story is how doctors took something simple – a blue dye that's been used safely in medicine for decades – and used it in a new, creative way. Instead of guessing where to operate, they could see exactly where the problem was. The result was a surgery that was faster, more precise, and gave the patient a complete recovery.
Think of it like using a special paint to highlight a crack in a wall before you fix it. The crack was always there, but now you can see it clearly and repair it perfectly.
Understanding Arteriovenous Malformations: When Blood Vessels Go Wrong
What Are Arteriovenous Malformations?
Think of your blood vessels like a city's road system. Arteries are like highways that carry fresh blood away from your heart to different parts of your body. Veins are like side roads that bring used blood back to your heart for cleaning. Normally, there are smaller roads called capillaries that connect the highways to the side roads smoothly.
An arteriovenous malformation, or AVM for short, is like having a highway connected directly to a side road without the proper connecting streets. This creates a traffic jam where blood flows too fast and in the wrong direction. The blood vessels get tangled up like a ball of yarn, and they become weak and prone to bleeding.
Why AVMs Are Dangerous
When blood vessels form these tangled clusters, several problems can happen:
Bleeding Risk: The twisted vessels are fragile and can break open, causing internal bleeding. This is like having a weak pipe that bursts under pressure.
Poor Blood Flow: Blood takes shortcuts through the AVM instead of going where it's needed. This means nearby tissues don't get enough oxygen and nutrients.
Growing Over Time: AVMs can get bigger as you age, making the problems worse. It's like a crack in a wall that keeps growing if you don't fix it.
Hidden Location: In the small intestine, AVMs are especially tricky because they're buried deep inside your body where doctors can't easily see or reach them.
Why Small Intestine AVMs Are Extra Challenging
The small intestine is about 20 feet long and folded up like an accordion inside your belly. It's responsible for absorbing nutrients from your food. When an AVM forms here, it can cause several specific problems:
Silent Bleeding: You might not know you're bleeding until you become very weak from blood loss. The blood might not be visible in your stool, making it hard to detect.
Chronic Anemia: Slow, steady bleeding can make you tired, weak, and pale because your body doesn't have enough healthy red blood cells.
Emergency Situations: Sometimes the AVM bleeds heavily all at once, which can be life-threatening and require immediate surgery.
Difficult Diagnosis: Finding a small AVM in 20 feet of twisted intestine is like finding a specific broken wire in a tangled bundle of cables.
Who Gets AVMs and Why?
AVMs can affect anyone, but they're more common in older adults. Some people are born with them, while others develop them over time. They're especially common in people over 50 and can account for 30-40% of all small intestine bleeding cases.
The exact cause isn't always clear, but factors that might contribute include:
- Age-related wear and tear on blood vessels
- Genetic factors that affect how blood vessels develop
- Other medical conditions that affect circulation
Signs That You Might Have an Intestinal AVM
The symptoms of an intestinal AVM can be subtle at first but tend to get worse over time:
Fatigue and Weakness: Feeling tired all the time, even after sleeping well
Pale Skin: Looking washed out or losing your normal color
Shortness of Breath: Getting winded from normal activities
Dark or Bloody Stools: Your bowel movements might look black, tarry, or have visible blood
Abdominal Pain: Cramping or discomfort in your belly
Need for Blood Transfusions: If bleeding is severe, you might need emergency blood replacement
The tricky thing about these symptoms is that they can be caused by many other health problems too. That's why finding the exact source of the bleeding is so important.
The Challenge of Finding Hidden Bleeding: Why Traditional Methods Often Fall Short
The Detective Work of Modern Medicine
When someone comes to the hospital with signs of internal bleeding, doctors become medical detectives. They know something is wrong, but they need to find exactly where the problem is hiding. This detective work becomes especially difficult when the bleeding is coming from the small intestine.
Why the Small Intestine Is So Hard to Examine
The small intestine presents unique challenges that make it one of the most difficult parts of the body to examine:
Length and Location: At about 20 feet long, the small intestine is folded and twisted deep inside your abdomen. It's like trying to examine a very long, winding tunnel that you can't easily access.
Between Two Areas: The small intestine sits between the stomach (which doctors can see with an upper endoscopy) and the large intestine (which they can see with a colonoscopy). It's in the middle zone that's hard to reach with traditional tools.
Delicate Structure: The walls of the small intestine are thin and sensitive. Pushing instruments through it requires great care to avoid causing more damage.
Constant Movement: Your intestines are always moving and shifting as they digest food. This makes it hard to get a clear, steady view of any one area.
Traditional Diagnostic Methods and Their Limitations
Before the methylene blue technique, doctors had several tools to find intestinal bleeding, but each had significant drawbacks:
Upper and Lower Endoscopy
What It Is: Doctors use a flexible tube with a camera to look inside the stomach (upper) or large intestine (lower).
The Problem: These tests often come back completely normal because they can't reach the small intestine where the AVM is hiding. It's like having flashlights that can only illuminate the beginning and end of a long, dark tunnel.
CT Scans and MRIs
What They Are: These imaging tests take detailed pictures of your insides from the outside.
The Limitations: Small AVMs might be too tiny to show up clearly on these scans. Also, if the AVM isn't actively bleeding during the test, it might be completely invisible. It's like trying to find a small leak in a pipe when the water isn't flowing.
Angiography
What It Is: Doctors inject contrast dye into your blood vessels and take X-ray pictures to see the blood flow.
The Challenge: This only works if the AVM is bleeding actively during the test. Many AVMs bleed on and off, so they might be quiet when the test is performed.
Capsule Endoscopy
What It Is: You swallow a pill-sized camera that takes pictures as it travels through your digestive system.
The Issues: While this can sometimes spot an AVM, it can't pinpoint the exact location for surgery. It's like knowing there's a problem somewhere in a 20-foot area but not knowing exactly where.
The Guessing Game of Surgery
Before the methylene blue technique, surgeons often had to make difficult choices:
Exploratory Surgery: Sometimes doctors had to open up the patient and examine the entire small intestine by hand, looking for clues. This meant much larger incisions and longer recovery times.
Educated Guessing: Based on test results, surgeons might have to guess where the AVM was located and remove larger sections of intestine than necessary.
Multiple Procedures: Patients might need several different tests and procedures before doctors could find and fix the problem.
Trial and Error: Sometimes the first surgery didn't find the bleeding source, requiring additional operations.
The Emotional and Physical Toll
For patients and families, this diagnostic uncertainty created significant stress:
Ongoing Symptoms: While doctors searched for answers, patients continued to experience bleeding, fatigue, and worry.
Multiple Hospital Visits: The search for a diagnosis often required many appointments, tests, and procedures.
Anxiety: Not knowing what was wrong or when it would be fixed caused tremendous emotional stress.
Physical Weakness: Continued bleeding left patients weak and sometimes requiring blood transfusions while waiting for a diagnosis.
The Need for a Better Solution
By the time doctors developed the methylene blue technique, it was clear that a new approach was desperately needed. The ideal solution would:
- Pinpoint the exact location of the AVM
- Work even when the AVM wasn't actively bleeding
- Allow for precise, limited surgery
- Reduce the number of procedures needed
- Give patients faster answers and treatment
This is exactly what the methylene blue technique was designed to accomplish, representing a major breakthrough in solving one of medicine's most challenging diagnostic puzzles.
The Methylene Blue Breakthrough: How a Simple Dye Solved a Complex Problem
What Is Methylene Blue?
Methylene blue is a bright blue dye that has been used safely in medicine for over 100 years. Think of it like food coloring for your body – it's safe, it shows up clearly, and it eventually gets filtered out by your kidneys. Doctors have used it for many different purposes, from treating certain poisonings to helping identify tissues during surgery.
The beautiful thing about methylene blue is that it's simple, affordable, and readily available in hospitals around the world. It's not a high-tech solution – just a smart way to use something that's been around for decades.
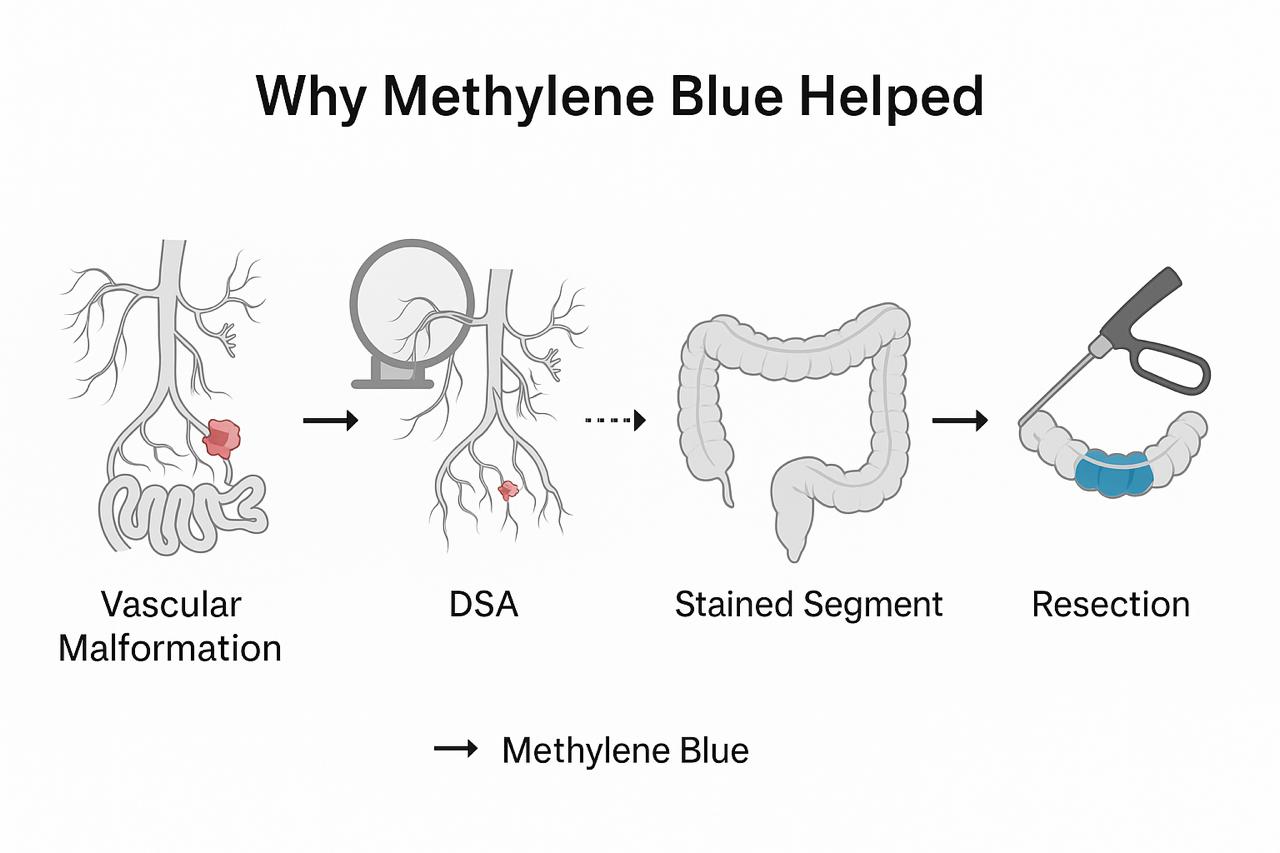
The Brilliant Idea Behind the Technique
The doctors who developed this technique had a clever insight: instead of trying to find a tiny AVM in 20 feet of intestine, why not make the AVM announce itself? By injecting methylene blue directly into the blood vessel that feeds the AVM, they could make that section of intestine turn bright blue, creating a clear target for surgery.
It's like using a highlighter to mark the important part of a long document. Instead of reading through 20 pages to find one crucial sentence, you can spot the highlighted section immediately.
Step-by-Step: How the Procedure Works
The methylene blue technique involves several coordinated steps that happen on the same day:
Step 1: Finding the Blood Vessel
First, doctors use a procedure called angiography to map out the blood vessels in the patient's abdomen. They insert a thin tube (called a catheter) through a small puncture in the groin and guide it up into the main artery that supplies blood to the small intestine.
This is like a plumber using a special camera to look inside pipes to find where they connect and branch off. The doctors inject contrast dye and take X-ray pictures to see the blood vessel network clearly.
Step 2: Identifying the Problem Area
Using the angiography images, doctors look for signs of the AVM. They're searching for areas where blood vessels look tangled or where blood flow appears abnormal. Sometimes they can see the AVM directly; other times, they identify which branch of the artery is most likely feeding the problem area.
This detective work is like following a trail of clues to narrow down the search area from the entire 20-foot small intestine to a much smaller section.
Step 3: Placing the Microcatheter
Once they identify the likely blood vessel, doctors thread an even thinner tube (called a microcatheter) through the main catheter. This microcatheter is incredibly small – thinner than a strand of spaghetti – and can be guided into very small blood vessels.
The skill required for this step is remarkable. It's like threading a needle while looking through a microscope, requiring years of specialized training.
Step 4: The Blue Dye Injection
Here's where the magic happens. With the patient already prepared for surgery, doctors inject methylene blue through the microcatheter directly into the blood vessel they suspect is feeding the AVM.
The blue dye flows through the blood vessel and into the surrounding intestine tissue. Within minutes, the section of intestine that contains the AVM turns a distinctive blue color, while the rest remains its normal pinkish color.
Step 5: Surgical Removal
With the target area clearly marked in blue, the surgeon can make a small, precise incision and remove only the affected section of intestine. There's no guesswork involved – the blue color shows exactly where to cut.
This is like having a clear boundary marked on a map. Instead of removing a large area “just to be safe,” the surgeon can remove just the necessary tissue, preserving as much healthy intestine as possible.
Step 6: Reconnection
After removing the blue-stained section containing the AVM, the surgeon reconnects the healthy ends of the intestine. The body is designed to heal these connections well, and the remaining intestine continues to function normally.
The Timing Is Everything
One of the most impressive aspects of this technique is the coordination required. The angiography team and the surgical team must work together seamlessly:
- The angiography is performed in a special room with X-ray equipment
- The patient is then quickly moved to the operating room
- The methylene blue injection happens just before the surgeon opens the abdomen
- The surgery must be performed while the blue dye is still visible
This coordination is like a well-choreographed dance between different medical specialists, each playing a crucial role in the success of the procedure.
Why This Approach Is So Effective
The methylene blue technique works so well because it solves the fundamental problem of localization:
Precision: Instead of guessing where the AVM is, surgeons can see exactly where it's located.
Minimal Tissue Removal: Only the affected area needs to be removed, preserving healthy intestine.
Single Procedure: Everything can be accomplished in one coordinated treatment session.
Reduced Risk: Smaller incisions and more precise surgery mean lower risk of complications.
Faster Recovery: Patients recover more quickly when less healthy tissue is removed.
The technique represents a perfect example of medical innovation – taking existing tools and using them in a new, creative way to solve a longstanding problem.
The Life-Changing Benefits: Why This Technique Is Revolutionary
Transforming Surgery From Guesswork to Precision
Before the methylene blue technique, removing an intestinal AVM was often like trying to fix a car engine while wearing a blindfold. Surgeons had to rely on educated guesses, general areas of suspicion, and sometimes pure luck. Now, it's like having a bright spotlight that illuminates exactly what needs to be fixed.
This transformation from guesswork to precision has created benefits that extend far beyond just finding the AVM – it has changed the entire experience for patients and their families.
Dramatic Reduction in Surgery Size and Trauma
Smaller Incisions, Faster Healing
Traditional exploratory surgery for intestinal bleeding often required large incisions that allowed surgeons to examine extensive sections of the intestine by hand. With the methylene blue technique, surgeons can make much smaller, more targeted incisions because they know exactly where to look.
Think of it like the difference between tearing down an entire wall to find a broken pipe versus making a small, precise hole exactly where the leak is located. The repair is the same, but the damage to the surrounding area is minimal.
Preserving Healthy Intestine
One of the most significant advantages is that doctors can remove only the diseased tissue while preserving all healthy intestine. Before this technique, surgeons often had to remove large sections of intestine “just to be safe,” which could affect digestion and overall health.
The small intestine plays a crucial role in absorbing nutrients from food. Removing more than necessary can lead to nutritional problems later in life. The precision of the methylene blue technique helps ensure that patients maintain optimal digestive function after surgery.
Eliminating the Need for Multiple Procedures
One-and-Done Approach
Many patients with intestinal AVMs previously faced a frustrating cycle of tests, procedures, and surgeries. They might have had:
- Multiple endoscopies that found nothing
- CT scans and MRIs that showed unclear results
- Angiography that missed the AVM because it wasn't bleeding
- Exploratory surgery that didn't locate the problem
- Additional surgeries to find what the first one missed
The methylene blue technique can often accomplish in one coordinated procedure what previously took multiple attempts over weeks or months.
Reduced Hospital Time
Instead of repeated hospital visits and extended stays for multiple procedures, patients can often have their problem diagnosed and treated in a single hospital admission. This means:
- Less time away from work and family
- Reduced medical costs
- Lower risk of hospital-acquired infections
- Less emotional stress from prolonged uncertainty
Immediate Visual Confirmation of Success
Seeing Is Believing
One of the most reassuring aspects of this technique is that everyone in the operating room can see exactly what's being treated. The bright blue staining makes it obvious to the surgeon, nurses, and any observers that they're removing the right tissue.
This visual confirmation provides several benefits:
- Surgeons can be confident they've removed all of the AVM
- There's clear documentation of what was treated
- The medical team can immediately see that the procedure was successful
- Patients and families can understand exactly what was done
Reducing Surgical Uncertainty
In traditional AVM surgery, there was always some uncertainty about whether the bleeding source had been completely removed. Surgeons might think they got it all, but couldn't be completely sure until the patient's recovery showed whether bleeding had stopped.
With methylene blue staining, the AVM tissue is clearly marked and completely removed in one procedure, dramatically reducing the chance that any diseased tissue is left behind.
Faster Recovery and Return to Normal Life
Minimal Disruption to Digestive System
Because the methylene blue technique allows for such precise tissue removal, patients typically experience:
- Less post-operative pain
- Faster return of normal bowel function
- Shorter recovery periods
- Fewer dietary restrictions after healing
- Lower risk of complications like bowel obstruction
Psychological Benefits
The precision and effectiveness of this technique also provide significant mental and emotional benefits:
Confidence in Treatment: Patients can be assured that their problem has been accurately identified and completely treated.
Peace of Mind: The visual confirmation of the procedure reduces anxiety about whether the treatment was successful.
Faster Resolution: Quick, effective treatment means less time living with uncertainty and worry about ongoing health problems.
Cost-Effectiveness for Healthcare Systems
While the methylene blue technique requires coordination between specialized teams, it often proves more cost-effective than traditional approaches:
Fewer Overall Procedures
- Eliminates the need for multiple diagnostic tests
- Reduces repeat surgeries
- Decreases total hospital days
Better Resource Utilization
- More efficient use of operating room time
- Reduced need for blood transfusions
- Lower complication rates mean fewer additional treatments
Long-term Savings
- Prevention of chronic anemia treatment costs
- Elimination of ongoing diagnostic expenses
- Reduced need for long-term monitoring
Setting a New Standard of Care
The success of the methylene blue technique has begun to influence how doctors approach other similar problems:
Innovation Inspiration
- Encourages creative use of existing medical tools
- Demonstrates the value of interdisciplinary cooperation
- Shows how simple solutions can solve complex problems
Teaching Tool
- Medical students and residents can clearly see what they're learning about
- The visual nature makes it an excellent educational technique
- Helps train the next generation of specialists
The methylene blue technique represents more than just a new procedure – it's a perfect example of how innovative thinking can transform medicine, making treatments more effective, less traumatic, and more reassuring for everyone involved.
Real Results: Patient Outcomes and Recovery Success Stories
The First Success Story That Changed Everything
The original case that demonstrated the power of the methylene blue technique involved a patient who had been struggling with mysterious intestinal bleeding. Like many people with hidden AVMs, this person had experienced the frustrating cycle of tests that found nothing and treatments that didn't work.
When doctors finally used the methylene blue technique, they were able to:
- Locate the AVM precisely using the blue staining
- Remove only a small section of intestine (about 4 inches)
- Complete the surgery quickly and safely
- Achieve complete healing with no complications
Most importantly, the patient remained completely free of bleeding during six months of follow-up care. This meant no more anemia, no more weakness, and no more worry about when the next bleeding episode might occur.
What Recovery Looks Like with This Technique
The First Few Days After Surgery
Patients who undergo the methylene blue technique typically experience a smoother recovery compared to traditional exploratory surgery:
Day of Surgery: Because the incision is smaller and more precise, patients often experience less post-operative pain and require fewer pain medications.
Days 1-3: Most patients begin eating light foods within 24-48 hours, as their digestive system returns to normal function more quickly.
Days 3-7: Many patients are able to return home within a week, compared to longer hospital stays often required after extensive exploratory surgery.
Returning to Normal Activities
The precision of the methylene blue technique means patients can typically return to their regular activities faster:
Week 1-2: Light activities and gradual increase in normal diet
Week 2-4: Return to work for most desk jobs and non-strenuous activities
Week 4-6: Most physical restrictions lifted, return to exercise and normal activities
Month 2-3: Complete healing and return to all normal activities
Long-Term Outcomes
The most encouraging aspect of the methylene blue technique is its long-term success rate:
No More Bleeding: Patients typically experience complete resolution of their bleeding problem because the entire AVM is removed in one procedure.
Preserved Digestive Function: Because only the diseased tissue is removed, patients maintain normal digestion and nutrient absorption.
No Recurrence: When the AVM is completely removed using precise localization, it doesn't grow back or cause future problems.
Measuring Success: What the Numbers Show
Bleeding Resolution Rates
Studies of patients treated with the methylene blue technique show impressive success rates:
- Complete bleeding resolution in the vast majority of cases
- No need for repeat procedures to find missed bleeding sources
- Significant improvement in blood counts and energy levels
- Elimination of the need for ongoing blood transfusions
Quality of Life Improvements
Patients report dramatic improvements in their daily lives:
Physical Improvements:
- Increased energy and stamina
- Better sleep quality
- Improved appetite and enjoyment of food
- Return to normal skin color and appearance
Emotional Benefits:
- Relief from anxiety about unpredictable bleeding
- Confidence in participating in normal activities
- Reduced fear of traveling or being far from medical care
- Overall sense of wellness and security
Reduced Healthcare Needs
After successful treatment with the methylene blue technique, patients typically require:
- Fewer doctor visits and lab tests
- No ongoing treatments for anemia
- Reduced need for emergency medical care
- Lower overall healthcare costs
Comparing Outcomes to Traditional Approaches
Surgery Time and Precision
Traditional Approach: Exploratory surgery often took 2-4 hours as surgeons examined large sections of intestine looking for the bleeding source.
Methylene Blue Technique: Surgery typically takes 1-2 hours because surgeons know exactly where to operate.
Amount of Intestine Removed
Traditional Approach: Surgeons often removed 12-24 inches of intestine to ensure they captured the bleeding area.
Methylene Blue Technique: Only 4-6 inches of clearly identified diseased tissue needs to be removed.
Success on First Attempt
Traditional Approach: Some patients required multiple surgeries because the bleeding source wasn't found or completely removed the first time.
Methylene Blue Technique: The visual confirmation typically ensures complete success in a single procedure.
Patient and Family Perspectives
Relief from Diagnostic Uncertainty
One of the most significant benefits reported by patients is the relief that comes from finally having a clear diagnosis and definitive treatment:
“For months, I knew something was wrong but nobody could tell me what it was. The methylene blue procedure not only fixed my problem but showed me and my family exactly what was being treated.”
Confidence in the Treatment
The visual nature of the methylene blue technique helps patients and families understand and trust their treatment:
“When the surgeon showed us the blue-stained tissue that was removed, we could see that they had found and fixed the exact problem. There was no question about whether the treatment worked.”
Return to Normal Life
Many patients describe the experience as getting their life back:
“I went from being tired and worried all the time to feeling completely normal. I can travel, exercise, and enjoy meals without worrying about bleeding.”
Factors That Contribute to Success
Early Detection and Treatment
Patients who receive treatment before developing severe anemia or complications tend to have the best outcomes and fastest recovery.
Skilled Medical Teams
The success of the technique depends on having experienced interventional radiologists and surgeons who can work together effectively.
Proper Patient Selection
The technique works best for patients with AVMs that can be identified on angiography and are accessible through blood vessel injection.
Comprehensive Follow-up Care
Regular monitoring after surgery ensures that healing is progressing normally and that no complications develop.
The methylene blue technique has transformed what was once a difficult and uncertain treatment into a reliable, successful procedure that gives patients their health and peace of mind back.
Being Realistic: Limitations and Important Considerations
Not a Universal Solution
While the methylene blue technique represents a major breakthrough, it's important to understand that it's not the perfect solution for every case of intestinal bleeding. Like any medical procedure, it has specific requirements and limitations that patients and doctors need to consider carefully.
Being honest about these limitations helps ensure that patients have realistic expectations and that the technique is used in the situations where it will be most helpful.
When the Technique Works Best
The Right Type of Problem
The methylene blue technique is specifically designed for arteriovenous malformations (AVMs) that can be seen on angiography. It works best when:
The AVM Is Visible: The blood vessel feeding the AVM must be identifiable on X-ray images taken during angiography.
The AVM Is Accessible: The blood vessel must be reachable with a microcatheter, which isn't always possible depending on the anatomy.
The AVM Is the Right Size: Very tiny AVMs might not take up enough dye to create visible staining, while very large ones might be obvious without special marking.
Patient Factors That Matter
Not every patient is a good candidate for this technique:
Overall Health: Patients need to be healthy enough to undergo both angiography and surgery in the same session.
Kidney Function: Since methylene blue is eliminated through the kidneys, patients with severe kidney disease might not be good candidates.
Allergies: Though rare, some people are allergic to methylene blue or the contrast dyes used in angiography.
Blood Vessel Anatomy: Some patients have unusual blood vessel patterns that make it difficult to navigate a microcatheter to the right location.
What Can Go Wrong
Technical Challenges
Even in experienced hands, several technical problems can occur:
Catheter Placement Issues: Sometimes the microcatheter can't be positioned correctly in the blood vessel feeding the AVM. This might happen due to:
- Unusual blood vessel anatomy
- Blood vessels that are too small or twisted
- Previous surgery that changed the normal anatomy
Dye Distribution Problems: The methylene blue might not distribute evenly, which could lead to:
- Weak staining that's hard to see during surgery
- Staining of healthy tissue in addition to the AVM
- Dye that washes out too quickly before surgery begins
Timing Coordination: The technique requires perfect timing between the angiography team and the surgical team. Problems can arise if:
- There are delays in moving the patient to the operating room
- The dye effect wears off before surgery begins
- Emergency situations interrupt the planned coordination
Medical Risks
While generally safe, the procedure does carry some risks:
Angiography Risks: The blood vessel catheterization can cause:
- Bleeding at the catheter insertion site
- Blood vessel injury or blockage
- Allergic reactions to contrast dye
- Kidney problems from the contrast material
Surgery Risks: Any intestinal surgery carries risks including:
- Infection at the surgical site
- Problems with healing at the connection points
- Temporary or permanent changes in bowel function
- General anesthesia complications
Methylene Blue Side Effects: Though uncommon, some patients may experience:
- Temporary blue discoloration of urine
- Mild allergic reactions
- Interaction with certain medications
When Alternative Approaches Might Be Better
Multiple AVMs
If a patient has several AVMs throughout their intestines, the methylene blue technique might not be the best choice because:
- It's designed to treat one specific location at a time
- Multiple procedures would be needed
- Other treatment approaches might be more practical
Very Small or Very Large AVMs
Tiny AVMs: Might not take up enough dye to be visible, making traditional endoscopic treatment more appropriate.
Large AVMs: Might be so obvious during surgery that special marking isn't necessary, and other approaches might be simpler.
Patients With Limited Life Expectancy
For patients with serious other health problems, less invasive treatments might be more appropriate than the coordinated angiography and surgery required for the methylene blue technique.
Hospital and Physician Requirements
Specialized Equipment and Expertise
Not every hospital can offer the methylene blue technique because it requires:
Advanced Imaging Equipment: High-quality angiography machines with microcatheter capabilities.
Experienced Specialists: Interventional radiologists skilled in complex catheter procedures and surgeons experienced in intestinal surgery.
Coordinated Teams: The ability to coordinate between different departments and specialties seamlessly.
Backup Plans: Resources to handle complications if they arise during the procedure.
Learning Curve Considerations
Even experienced physicians need time to master this technique:
- The first few cases at a new center might take longer
- Teams need practice coordinating their efforts
- Patient selection improves with experience
Cost and Insurance Considerations
Procedure Costs
The methylene blue technique can be expensive because it involves:
- Specialized angiography equipment and staff
- Operating room time for surgery
- Coordination between multiple medical teams
- Potential for longer hospital stays if complications occur
Insurance Coverage
Coverage for this technique may vary:
- Some insurance companies readily cover it as an established procedure
- Others might require pre-authorization or consider it experimental
- Patients should check with their insurance provider before proceeding
The Importance of Realistic Expectations
Success Isn't Always Immediate
While the methylene blue technique has high success rates, patients should understand that:
- Complete healing takes time, just like any surgery
- Some patients might need additional monitoring or treatment
- Recovery experiences vary from person to person
Not Every Case Is Straightforward
Some patients will have more complex situations that require:
- Modified surgical approaches
- Additional procedures
- Longer recovery periods
Making Informed Decisions
Patients considering the methylene blue technique should:
Ask Detailed Questions: Understand exactly what the procedure involves and what the expected outcomes are in their specific situation.
Consider All Options: Discuss alternative treatments with their healthcare team to make sure they're choosing the best approach.
Understand the Risks: Be fully informed about what could go wrong and how complications would be handled.
Have Realistic Timeline Expectations: Understand that this is major surgery with a real recovery period, even though it's more precise than traditional approaches.
The methylene blue technique represents a significant advance in treating intestinal AVMs, but like all medical procedures, it's not perfect for every situation. The key is working with experienced healthcare providers to determine if it's the right choice for each individual patient.
Looking Forward: The Future of Medical Innovation and Hope for Patients
A Simple Solution That Changed Everything
The story of the methylene blue technique is really a story about how medical breakthroughs happen. It wasn't developed in a high-tech laboratory using expensive new equipment or revolutionary discoveries. Instead, it emerged from doctors who took a step back, looked at an old problem in a new way, and found a creative solution using tools that had been available for decades.
This represents the best of medical innovation – not always the most expensive or complicated solution, but often the most clever and practical one.
What This Means for Future Medical Discoveries
The Power of Creative Thinking
The methylene blue breakthrough demonstrates that some of the most important medical advances come from asking different questions:
- Instead of “How can we build better tools to find AVMs?” the researchers asked “How can we make AVMs show themselves?”
- Instead of “How can we remove more tissue safely?” they asked “How can we remove only exactly what needs to be removed?”
This type of creative problem-solving suggests that many other medical challenges might have simpler solutions than we initially think.
Building on Existing Knowledge
The technique shows how powerful it can be to combine existing medical procedures in new ways:
- Angiography had been used for decades to see blood vessels
- Methylene blue had been used safely in medicine for over 100 years
- Intestinal surgery was already well-established
The breakthrough came from putting these pieces together in a coordinated, innovative way.
The Importance of Teamwork
Perhaps most importantly, this technique demonstrates that the future of medicine often lies in better cooperation between different specialists. The success of the methylene blue approach required:
- Interventional radiologists who could navigate tiny blood vessels
- Surgeons skilled in intestinal procedures
- Anesthesiologists who could coordinate care between two procedures
- Nurses and technicians who could facilitate smooth transitions
Expanding Applications and Future Possibilities
Other Types of Bleeding
Researchers are already exploring whether similar dye techniques could help locate bleeding sources in other parts of the body:
- Other areas of the digestive system
- Blood vessel problems in the lungs or kidneys
- Bleeding sources that are hard to find during surgery
Different Types of Dyes
Scientists are investigating whether other safe dyes might work even better than methylene blue:
- Dyes that last longer, giving surgeons more time
- Dyes that show up more clearly under special lights
- Dyes that can mark different types of tissue problems
Combination Approaches
Future developments might combine the methylene blue technique with other advanced technologies:
- Real-time imaging during surgery to see dye distribution
- Robotic surgery tools that can work more precisely with dye marking
- Advanced anesthesia techniques that make the coordination even smoother
Hope for Patients Facing Similar Challenges
Faster Diagnosis and Treatment
The success of this technique gives hope that other diagnostic challenges in medicine might have simpler solutions than we currently realize. Patients who are facing mysterious symptoms or difficult-to-diagnose conditions can take encouragement from the fact that medical innovation continues to find new ways to solve old problems.
Less Invasive Treatments
The trend toward more precise, less invasive treatments continues to improve patient experiences. The methylene blue technique is part of a larger movement in medicine toward:
- Smaller incisions and faster healing
- Treatments that preserve as much healthy tissue as possible
- Procedures that can be completed in single sessions
Better Quality of Life
Perhaps most importantly, innovations like this demonstrate that medical advances can dramatically improve not just survival, but quality of life. Patients don't just want to live – they want to live well, without ongoing symptoms, restrictions, or worry.
The Ripple Effects of Innovation
Training the Next Generation
The methylene blue technique has become an important teaching tool in medical schools and residency programs. Young doctors learning about this approach are being trained to think creatively about problem-solving and to value precision over guesswork.
Inspiring Further Research
Success stories like this one often inspire researchers to tackle other challenging problems with renewed energy and optimism. When the medical community sees that creative solutions can work, it encourages more innovative thinking across many different areas.
Improving Medical Confidence
When patients and families see that medicine can solve problems that previously seemed impossible, it increases trust and confidence in healthcare. This can lead to earlier treatment-seeking, better compliance with medical recommendations, and improved outcomes overall.
A Personal Message of Hope
For anyone reading this who is facing a medical challenge that seems overwhelming or mysterious, the methylene blue story offers several important messages:
Innovation Never Stops: Medical researchers and doctors are constantly working to find better ways to diagnose and treat health problems.
Simple Solutions Exist: Sometimes the answer to a complex problem is simpler than anyone expected. Don't lose hope if current approaches aren't working.
Teamwork Matters: The best medical care often comes from teams of specialists working together. Don't hesitate to seek care at centers where different experts can collaborate on your behalf.
Your Problem Matters: Even if your condition seems rare or difficult, researchers and doctors are working on solutions. Today's impossible problem could become tomorrow's routine treatment.
The Broader Lesson
The methylene blue technique teaches us that medical progress often comes not from dramatic breakthroughs, but from thoughtful innovations that make existing treatments work better. It reminds us that the most important advances in medicine are often measured not in technological complexity, but in improved outcomes for real people facing real health challenges.
In a world where medical news often focuses on expensive, high-tech solutions, the methylene blue story offers a refreshing reminder that sometimes the best innovations are the simplest ones – and that creative thinking, combined with compassionate care, continues to make the impossible possible.
This technique has given patients their lives back, given families peace of mind, and given the medical community a model for how innovation should work: effectively, safely, and with the patient's wellbeing as the ultimate goal.
Related: Healthletic Methylene Blue